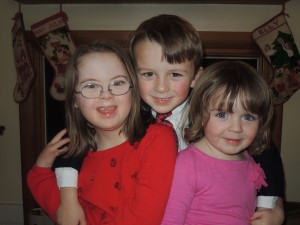
In the midst of this month’s conversation about potential new treatments for people with Down syndrome and the possibilities, problems, and questions those treatments raise, I thought it was important to offer a summary of the research and its implications. To that end, I asked Dr. Faycal Guedj, a researcher at Tufts University who has been working on these new treatments, to provide an overview. Dr. Guedj also has a 25-year old sister with Down syndrome, so he approaches the subject from both a clinical and personal perspective.
My hope for this series is to collect an array of voices, and to start a civil conversation among people who disagree with one another so that we might all learn together. Yesterday we heard from Rachel Adams, who wrote about The Damaging Language of “Cure” and Down Syndrome. Although Dr. Guedj does not use the language of cure, he does offer a different perspective than Adams. In both cases, I hope you will read, reflect, comment, ask questions, and do so with respect even (especially) if you disagree. My questions to Dr. Guedj appear at the end of this essay. Now, Faycal Guedj writes:
Fifty years after the discovery of the chromosomal origin of Down syndrome (DS) as being the presence of three copies of chromosome 21 (HSA21), lots of mysteries around the pathophysiololgy of this disease have been uncovered. During this period, DS research went through three major steps: 1) The identification and sequencing of HSA21 genes; 2) The creation and characterization of mouse models to study these genes; 3) The development of therapeutic strategies mostly to improve cognition in young adults.
In the year 2000, the sequencing of the HSA21 was completed and close to 250 genes were identified. Understanding the role of all these genes individually is a major challenge and hardly achievable, however, the presence of rare cases of partial trisomy 21 led to the discovery of candidate chromosomal regions containing a small number of genes strongly associated with some DS phenotypes. The first region called DS critical region (DSCR) contains 20 genes responsible for the cognitive delay and the craniofacial features of DS. The second region or the DS congenital heart defect region (DSCHD) contains 33 genes, and includes the DSCR.
At the same time, technical advances in genetic manipulation of mice have had a great impact on the achievements of the DS research community in the last two decades. We took advantage of the similarities between the human and mouse genomes to create several mouse models carrying a trisomy of either a single gene such as DYRK1A, SOD1, APP (monogenic models), or chromosomal regions (partial trisomy models), including the Ts65Dn and Ts1Cje models. These models contributed enormously in increasing our knowledge of the cellular and molecular origins of different clinical traits of DS, and still offer the most reliable and effective systems to test therapeutic interventions before proceeding to human clinical trials.
To improve cognition in DS, researchers have chosen two major therapeutic strategies. The first strategy targets single candidate genes like Dyrk1A using specific a non-toxic inhibitor (Epigallocatechine gallate or EGCG, a green tea polyphenol). This approach gave very promising results in the mouse and led to a pilot clinical trial. The second therapeutic approach aims to normalize the imbalance observed in some networks affected in the brain of DS patients, including oxidative stress, GABA transmission, serotonine and acetylcholine networks as well as neuroinflammation. Around 20 molecules were tested on the Ts65Dn mice, and most of them were reported to significantly enhance learning and memory in this model.
Despite the positive effects in the mouse studies, a very limited number of human clinical trials were conducted mostly on young adults with DS. Piracetam, donepezil and rivastigumine (three of them target acetyl choline pathway), memantine (targets neuroinflammation and NMDAR), vitamin E (targets oxidative stress), folinic acid and growth hormone failed to significantly improve cognitive performances in double-blinded clinical trials. More recently, a pilot clinical trial using EGCG-rich green tea extract (inhibitor of DYRK1A) demonstrated that treated individuals have higher accuracy in visual memory recognition and spatial working memory, suggesting a positive effect of this compound both on the hippocampal and prefrontal systems. A larger (130 affected young adults) and more sophisticated clinical trial is being conducted in France and Spain to confirm this therapeutic benefit of EGCG.
Now, what future for the DS research in the next 10 years?
The recent development and clinical use of non-invasive prenatal testing (NIPT) techniques will probably impose a huge shift in DS research towards a prenatal treatment approach. It is well established that DS is a developmental disease and most its clinical manifestations are emerging during fetal life and shortly after birth until childhood. An early diagnosis of trisomy 21 with NIPT (10 weeks of gestation) offers a tremendous opportunity to intervene in utero using safe and well-designed therapeutic strategies that will potentially lead to a very significant, which is not to say a complete, normalization of brain development and cognitive outcome in newborns and children affected with DS.
In such an approach, three major challenges emerge in identifying compounds that (1) are safe for pregnant women and their fetuses, (2) can cross the placenta to achieve therapeutic levels in the fetus, and (3) show evidence of clinical improvement after birth.
A new era has started in DS research: Multidisciplinary teams need to be formed with a combination of geneticists, neuroscientists, clinicians, pharmacologist, toxicologist, families and parents advocate groups to resolve these challenges, and get the necessary expertise and support in order to provide effective treatments and guidelines to the national and international DS community.
In the Mother Infant Research Institute (Tufts Medical Center, Boston), we started, with Drs. Diana Bianchi and Tomo Tarui, a multidisciplinary collaborative effort that brings together the word-known expertise of Dr. Tarik Haydar (Boston University, Boston), Dr. Jeroen Pennings (National Institute for Public Health and the Environment, The Netherlands) and Dr. Donna Slonim (Tufts University, Boston) to develop effective prenatal treatments using a rigorous approach. We combine the study of human amniotic fluid and amniocytes obtained from DS pregnancies and the brains of several mouse models, including Ts65Dn and Ts1Cje to identify several candidate and FDA-approved drugs that will be extensively tested during the next 3-5 years in vitro and in vivo with potential clinical trials during this period.
This collaborative effort will need an important financial support by the DS community, foundations and public health funding agencies, and could be translated to develop therapies for other conditions, including other neurodevelopmental diseases (trisomy 18, autism, fragile-X) and neurodegenerative conditions (Alzheimer and Parkinson disease).
I strongly believe, now more than ever, that the lives of these kids will change for the best, and that humanity will benefit from their high social skills to improve our world.
My final thought goes to my sister, Imene, affected with DS and who is 25 years old: “I wish that you were born just now, your life would have been so different!!! I LOVE YOU MORE THAN ANYTHING ON EARTH”.
Faycal Guedj, a brother of a sister with DS.
Upon reading, I asked Dr. Guedj to answer a few further questions:
Would you expect these therapeutic interventions to change the physical effects of DS in addition to the cognitive? For instance, would you expect fewer instances of heart defects and/or less severe defects?
Answer: I didn’t want to dive into complicated details for your readers, but I suspect that a well-designed prenatal treatment will positively impact not only the brain development but also the heart and the thymus. In DS patients, the development of these organs is perturbed by the expression increase of some chromosome 21 genes, which induce imbalance in some pathways (NFAT pathway is an example). This pathway is very active in the brain, heart and thymus during fetal development and we can imagine that targeting it with a particular drug will improve cognition but also decrease the severity of heart and thymus defects. An effective treatment will need to be associated with extensive learning programs, speech and physical therapies to potentiate its effect.
On the more philosophical level, I think many of my readers do not assume that higher IQ is necessarily good. You imply that improved cognition is of course a good thing, and I wonder if you can explain why researchers see such positive gains as a result of improved cognition.
Answer: Cognition stands for a set of intellectual performances including IQ, learning, memory, speech development, reading, writing, behavior The bottom line is that improving cognition will help individual with DS to live an autonomous life. I think that it will be a huge achievement for families. As you know, we are always asking ourselves this big question: How my kid will be living when I am gone?. Every parent of a kid with Down syndrome thinks about this all the time, and probably improving the independent life skills of these kids is one part of the answer.
One final point of clarification– do you think Imene would live a better life now due to this type of research or due to advances we have made as a culture or both?
Answer: I believe that my sister will benefit from these advances and that her life quality will improve dramatically. However, it is well known that the brain of the fetus, the baby and the child are still actively developing, and that the earlier we treat, the more efficiently will we improve the cognitive outcome in our kids.
Dr. Faycal Guedj received his Ph.D. in neuroscience and human genetics from the University of Paris. He did his postdoctoral research at Tufts University where he continues to work on questions related to treatments for individuals with Down syndrome.