Three items:
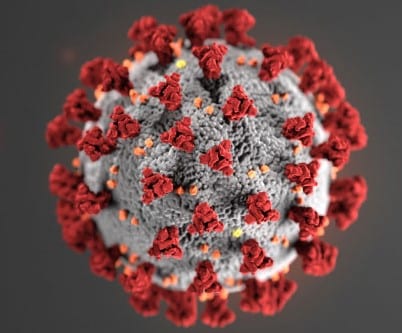
First, Cycle Thresholds.
In the New York Times this past weekend: “Your Coronavirus Test Is Positive. Maybe It Shouldn’t Be.”
The article explained that PCR testing is not merely a yes-or-no on coronavirus infection, but that it measures the viral load. In particular, “number of amplification cycles needed to find the virus, called the cycle threshold” is crucial information because a higher threshold identifies people as testing positive who have extremely tiny viral loads and are not infectious. The Times reported,
On Thursday, the United States recorded 45,604 new coronavirus cases, according to a database maintained by The Times. If the rates of contagiousness in Massachusetts and New York were to apply nationwide, then perhaps only 4,500 of those people may actually need to isolate and submit to contact tracing.
One solution would be to adjust the cycle threshold used now to decide that a patient is infected. Most tests set the limit at 40, a few at 37. This means that you are positive for the coronavirus if the test process required up to 40 cycles, or 37, to detect the virus.
Tests with thresholds so high may detect not just live virus but also genetic fragments, leftovers from infection that pose no particular risk — akin to finding a hair in a room long after a person has left, Dr. Mina said. . . .
A more reasonable cutoff would be 30 to 35, she added. Dr. Mina said he would set the figure at 30, or even less. Those changes would mean the amount of genetic material in a patient’s sample would have to be 100-fold to 1,000-fold that of the current standard for the test to return a positive result — at least, one worth acting on. . . .
Officials at the Wadsworth Center, New York’s state lab, have access to C.T. values from tests they have processed, and analyzed their numbers at The Times’s request. In July, the lab identified 794 positive tests, based on a threshold of 40 cycles.
With a cutoff of 35, about half of those tests would no longer qualify as positive. About 70 percent would no longer be judged positive if the cycles were limited to 30.
In Massachusetts, from 85 to 90 percent of people who tested positive in July with a cycle threshold of 40 would have been deemed negative if the threshold were 30 cycles, Dr. Mina said. “I would say that none of those people should be contact-traced, not one,” he said.
This is huge. But in the week that followed, I had not seen any follow-up reporting. Heck, I sent off an e-mail to the press folks at the Illinois Department of Health asking about this and am still waiting for a response.
And this isn’t just about raw numbers of diagnosed cases. After all, in Illinois, we’ve seen cases increasing — gradually to be sure — from their low of 409 on June 16 (implied infections calculated at rt.live, which does the math around testing volume) to a Sept. 2 figure of 899, a 120% increase; while hospitalizations and deaths have remained steady or only moderately increased — 1,385 on July 6 as a rolling 7 day average, to 1543 on Sept. 2, a 12% increase; and with deaths per day hovering in the upper teens for all of July and August. The explanation has generally been that it is young people now getting infected and that, with enough lag time, they will infect their parents — but two months is quite a bit of lag time. If in fact, Illinois uses the cycle threshold of 40, or 35, and if the an increasing proportion of those new cases are ones which would not have been deemed positive under a lower cycle threshold, this is important information to help us understand what is truly going on — and how that impacts the political decisions being made by Pritzker and by local school boards.
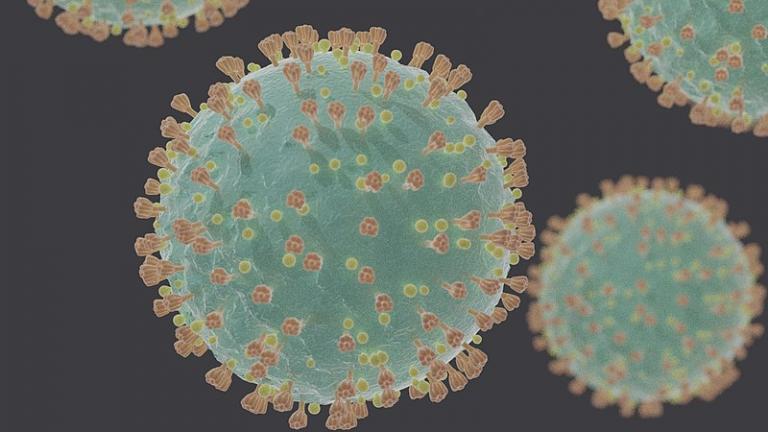
Second, Vitamin D.
There was speculation a while back that vitamin D deficiency caused one to be more susceptible to Covid. I don’t know if initially this was due to preliminary research or just the observation that populations more likely to be vitamin D deficient appeared to be more affected. (Darker skin doesn’t absorb as much from the sun; people in countries at northern latitudes are more accustomed to vitamin D supplements; milk-drinkers get vitamin D through their milk, etc.) But then a study refuted that speculation and my efforts to take my daily multivitamin tanked. Now the Chicago Tribune has a report that this study was poorly designed and a better-designed study confirms the vitamin D link spectacularly: “Lack of vitamin D might increase risk for COVID-19, University of Chicago researchers find.”
Researchers looked at 489 patients tested for COVID-19 at University of Chicago Medicine between March 3 and April 10, whose vitamin D levels had been measured within a year of being tested for COVID-19.
Patients with untreated vitamin D deficiencies were 77% more likely to test positive for COVID-19 as patients with sufficient levels of the vitamin, according to the research, which was published Thursday in the peer-reviewed journal JAMA Network Open. The findings were reported earlier this year before the study was officially published.
“It raises the possibility that if you take vitamin D, you might be less likely to catch COVID,” said Dr. David Meltzer, chief of hospital medicine at University of Chicago Medicine and lead author of the study. “It’s very inexpensive. It could be used very broadly.”
The article documenting the study is also available in open-access format. According to this, the initial data collection took place very early, in the grand scheme of things: patients tested for covid at the University of Chicago Medicine from March 3 to April 10; this means this was at a point at which testing was limited to “persons presenting with potential symptoms of COVID-19 admitted to the hospital or health care workers with COVID-19 symptoms and exposure.” They matched these patients with existing health records for these patients, to identify whether they had been vitamin D deficient. Because the University of Chicago is on the south side of Chicago, a significant proportion of their patients were Black/African American or nonwhite more generally speaking.
Here are some of the stats:
Percent Black/African American: 58%
Percent nonwhite: 68%
Percent vitamin D deficient: 35% (this seems very high but I would guess that at least some of these patients were tested not as part of routine blood testing but because of symptoms suggesting deficiency).
Of white patients: 19%
Of nonwhite patients: 43%
Of total population:
Percent testing positive for covid: 15%
Percent testing positive, among those with vitamin D deficiency: 19%
Percent testing positive, without deficiency: 12%.
The paper’s authors then suggest that vitamin D supplementation might be a low-cost way to reduce covid-19 incidence, especially for groups with high rates of vitamin D deficiency, that is, people of African and Latin American origin.
So, on the one hand, this is very encouraging. On the other hand, it is disappointing that we’re half a year into the pandemic before someone says, “hey, take vitamin D as a preventative.” I don’t know how much of the delay, in this particular case, was because it simply took a lot of time to pull together the data, or whether it’s a matter of the peer review process. I know there’s a balance between getting results out quickly enough to make a real difference to people’s lives as soon as possible, and getting the science right (see: stem cell treatments for breast cancer) but it is frustrating to think that the strong emphasis on “social injustice is the cause for the worse impact of covid on racial/ethnic minorities in the US” could have played a role in holding back science that would show that there were physiological differences at work.
Which brings me to
Sickle Cell Disease
and an article at Stat, “Millions of Americans carry the sickle cell trait, many without knowing it. Could they be at risk for severe Covid-19?” which begins:
Sckle cell disease, which causes Covid-like symptoms — clotting, strokes, and severe oxygen deprivation — is one of the medical conditions that the Centers for Disease Control and Prevention says puts people at higher risk for severe illness from the coronavirus. Now, a research team is trying to determine whether the several million people who merely carry one copy of the sickle cell mutation — but do not have the disease itself — could be more vulnerable to Covid-19, and whether that might be one reason the virus is disproportionately sickening and killing Black Americans.
About 100,000 Americans have sickle cell disease, an inherited disorder marked by sickle-shaped blood cells that can clump together, causing painful blockages of blood vessels, strokes, anemia, and early death. According to the American Society of Hematology, up to 3 million Americans may have the sickle cell trait, meaning they carry one copy of the gene — often without knowing it. (Two copies are required to have the disease.) In the U.S., both the disease and the trait largely affect African Americans.
Now, the article is not reporting on any completed research but a study that is currently underway. And note this:
Ethnicities with a high prevalence of sickle cell trait . . . include not just African Americans, but also Latin Americans from Central and South America and people of Middle Eastern, Asian, Indian, and Mediterranean descent.
This is, of course, because the sickle cell trait is somehow connected up with protection against malaria. It’s the same sort of thing as thalassemia in places like Italy and Greece, which a friend suggested was connected a while back.
So, again, how would it change our perceptions if this study found another physiological reason for ethnic minorities to be more at-risk of covid?