The 1 Nov edition of American Family Physician features a particularly thorny case study:
A 44-year-old female patient, who is a native of Africa, recently came to the United States to join her son, who is a naturalized U.S. citizen. She does not speak English, but my clinic has a staff member fluent in her native language. Through this interpreter, the medical staff obtained a history of urinary bladder problems that have persisted for at least three months. After detailed questioning, I learned that her symptoms were chronic pain and frequent, urgent urination.
After further questioning, the doctor was worried that the patient had bladder cancer, and may need urgent treatment. The only way to obtain a correct diagnosis was by a proper examination. But when the doctor suggested this, she refused:
I communicated my clinical concern to the patient, but she continued to refuse further examination such as cystoscopy. She indicated that her religious beliefs did not allow such “intimate” exposures.
So this patient potentially had a life-threatening, treatable condition. But her religious beliefs dictated that she would rather die than get a proper diagnosis and treatment. What would you do in this situation? Here’s what the doctor concerned recommends:
First off, he points out that giving up and discharging the patient is not an ethical option (medical professionals, he says, are subject to some degree of “obligatory beneficence”).
Second, he considers alternative diagnostic procedures, but concludes there aren’t any that will be conclusive.
As a last resort, he proposes to call in a religious authority, in an effort to persuade the patient to be sensible. But this seems potentially hazardous (because such individuals have no relevant training and may not have any relevant patient skills at all), not to mention morally problematic (after all, it was the religious clergy that caused the problem in the first place).
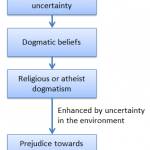
So what are the other options? After all, the real problem here is that this woman has been brainwashed with a set of primitive and dangerous beliefs, beliefs that have no basis in reality. The bottom line is that this is a psychiatric problem. Normally, patients with psychiatric problems are referred to psychiatrists, not to co-delusionists who may well reinforce their delusions.
What’s more, this case is an example of the burdens placed on society by religion:
The clinical realities and language interpretation needed in this scenario would require several hours for resolution and understanding. Few medical institutions are staffed for this type of difficult communication.
The UK National Health Service currently spends some £20 million annually on religious service providers. Perhaps we would get greater benefit from spending that money on social and psychiatric services?
Ref: English DC. Addressing a patient’s refusal of care based on religious beliefs. Am Fam Physician. 2007 Nov 1;76(9):1393-4.