Valuable for pastors.
A recent RadioLab podcast, titled The Bitter End, identified an interesting paradox. When you ask people how they’d like to die, most will say that they want to die quickly, painlessly, and peacefully… preferably in their sleep.
But, if you ask them whether they would want various types of interventions, were they on the cusp of death and already living a low-quality of life, they typically say “yes,” “yes,” and “can I have some more please.” Blood transfusions, feeding tubes, invasive testing, chemotherapy, dialysis, ventilation, and chest pumping CPR. Most people say “yes.”
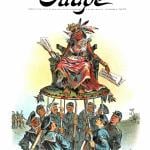
But not physicians. Doctors, it turns out, overwhelmingly say “no.” The graph below shows the answers that physicians give when asked if they would want various interventions at the bitter end. The only intervention that doctors overwhelmingly want is pain medication. In no other case do even 20% of the physicians say “yes.”…
The paradox, then — the fact that people want to be actively saved if they are near or at the moment of death, but also want to die peacefully — seems to be rooted in a pretty profound medical illiteracy. Ignorance is bliss, it seems, at least until the moment of truth. Physicians, not at all ignorant to the fraught nature of intervention, know that a peaceful death is often a willing one.